Moxibustion, to correct a breech presentation of the fetus
What problem does it solve?
It is known that when a fetus presents in the breech position and a caesarean section is not performed, perinatal morbidity is 12 times greater, and perinatal mortality is 3 times greater than in normal presentation.
In a recent multicentre trial carried out in 26 countries on a sample of 2083 women, perinatal and neonatal mortality and serious neonatal morbidity were significantly lower in the group with caesarean deliveries than in the group with vaginal deliveries (Hannah, 2000). From the 1970s on, in both Europe and America, breech births by vaginal delivery were declining and being replaced by caesarean deliveries. In some countries, replacement reached 90–100%. In Tuscany (Italy) in 1999, out of 1,058 breech presentations, there were 66 vaginal deliveries (6.2%), 987 caesarean births (93.2%) and one delivery with the aid of a ventouse (in 4 cases, the kind of birth was not recorded).
Not all authors agree on the generalised choice of a caesarean delivery in cases of breech presentation because they consider that this technique has not improved neonatal prognosis and has increased the risk of complications for the mother.
The frequency of breech presentation varies according to the stage of pregnancy. It is more frequent at the earlier stages (20-25% in the 28th week, 12% in the 31st–32nd week, and 7% at the 35th), whilst the frequency at term falls to 3–4% (Curiel P. 1996).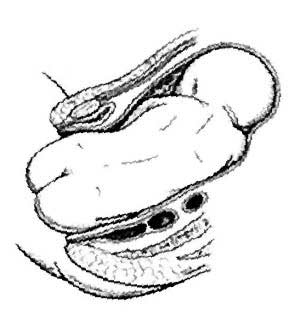
The causes of breech presentation at term are known in only 15% of cases and are due to uterine, pelvic and fetal anomalies, reduction of the amniotic fluid or the presence of fibroids (Curiel P. 1996; Hughey MJ. 1985).
In 1985 Westgren and other authors conducted a prospective survey in which an ultrasound scan was used to assess fetal position in the 32nd week of 4,600 pregnancies. In 310 cases the fetus was in the breech position. The progress of these 310 pregnancies were then followed with a weekly ultrasound scan until the time of birth to monitor the spontaneous version of the fetus. The fetus turned spontaneously in about 46% of the primagravidas, in 32% of the multigravidas with a previous breech delivery and in 78% of the multigravidas with no history of a breech delivery.
As an alternative to a caesarean section, an external cephalic version (ECV) is generally recommended to turn the fetus. The success rate of this technique varies according to author and case histories. The positive data given in the literature vary from 41% (74 cases examined) to 97% (30 cases) concentrated nevertheless around 60-70% in studies on a higher number of cases.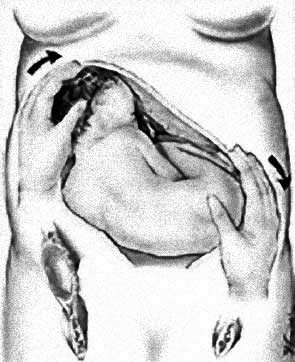
Generally, external cephalic version cannot be carried out before the 36th–37th week, with some contraindications such as multiple pregnancy, placenta previa, uterine bleeding, fetal malformations, rupture of the amniotic sac, an anomalous cardiotocograph, diabetes and maternal hypertension, oligohydramnios, a previous hysterotomy, and retarded growth. The success rate is influenced by gestational age, parity, the quantity of amniotic fluid, the position of the placenta (more successful in the fundic or lateral position), the degree of entry of the breech, fetal weight, type of presentation, position of the fetus’ back, and amount of maternal abdominal fat.
Nevertheless some authors have some reservations about the use of external cephalic version related to possible complications such as detachment of the placenta, premature rupture of the membranes, knotting of the umbilical cord, uterine bleeding, and the reduction of the fetal heartbeat. When it is transitory, this latter event is not considered to be a complication by other authors who consider it a response to the momentary reduction of the utero-placentary flow. The possibility that complications may arise, independently of their frequency, means that external cephalic version must be performed in a hospital equipped to deal with an urgent caesarean section if necessary.
In economic terms, the caesarean sections cost more than vaginal deliveries. While a patient who has had a normal birth is usually discharged on the second or third day, a woman who has had a caesarean section may have to stay in hospital for up to 15 days. The social costs of a generally traumatic event for the mother and her family and the organisational problems that may be caused by a long stay in hospital must also be taken into account. Furthermore, in countries where hospital conditions are not very good, women in labour are exposed to the risk of contracting other diseases, in particular post-operative infections.
For these reasons, it is extremely important to find practical and sustainable solutions to avoid the need for caesarean deliveries in the case of breech presentation.
One possible solution is the use of acupuncture and, in particular, moxibustion.
In a controlled clinical randomised open trial conducted in China (Cardini et al. 1998), the efficacy of moxibustion was evaluated in 260 women with breech presentation in the 33rd week and compared with a control group who did not receive this treatment. In the 35th week the success rate was 75% in the intervention group, while in the control group 48% of the fetuses were in the vertex position. Although 24 women in the control group and one woman in the intervention group underwent ECV, at the time of birth 75% of the intervention group were cephalic against 62% of the control group. The difference between the two groups is statistically significant.
At the moment, randomised clinical trials are under way in the West and these are producing results that partially overlap those obtained in China, with significantly higher effectiveness rates compared with the control group, even if the results of the trials carried out on Chinese women gave better results. The difference is probably due to different cultural attitudes in the East where this kind of treatment is widely accepted.
DOWNLOAD THE BROCHURE PDF
albanian (0.7 MB)english (0.4 MB)
spanish (0.4 MB)
serbian (0.9 MB)






 COUNTRY OF ORIGIN
COUNTRY OF ORIGIN